Mpox Guidance for Healthcare Providers
To report a positive laboratory result for orthopox or mpox virus, immediately call the Communicable Disease Program at (209) 558-5678 during business hours: Monday-Friday, 8AM-5PM, or send an email to CDNurse@schsa.org
Testing and Specimen Submission
Healthcare providers should be alert and consider mpox virus in patients who present with an unexplained rash or lesions consistent with mpox:
- Instruct patient to isolate and avoid contact with other people while waiting for test results
- Submit specimens for mpox testing through commercial laboratories if possible. A list of commercial laboratories providing mpox testing is available at CDPH's Information for Health Care Providers Page
- Treatment with Tecovirimat (TPOXX)
Please check with reference lab regarding their lab-specific submission forms and requirements for specimen collection, labeling, and transport.
There is no need to contact Stanislaus County Public Health for approval to test at commercial laboratories. Providers are required to report all suspected and confirmed cases to Stanislaus County Public Health within 1 working day.
Under certain circumstances, Public Health will directly process specimens using our own labs. This includes if the person suspected to have mpox is pregnant, if they are a health care worker, or if an outbreak is identified in a specific location.
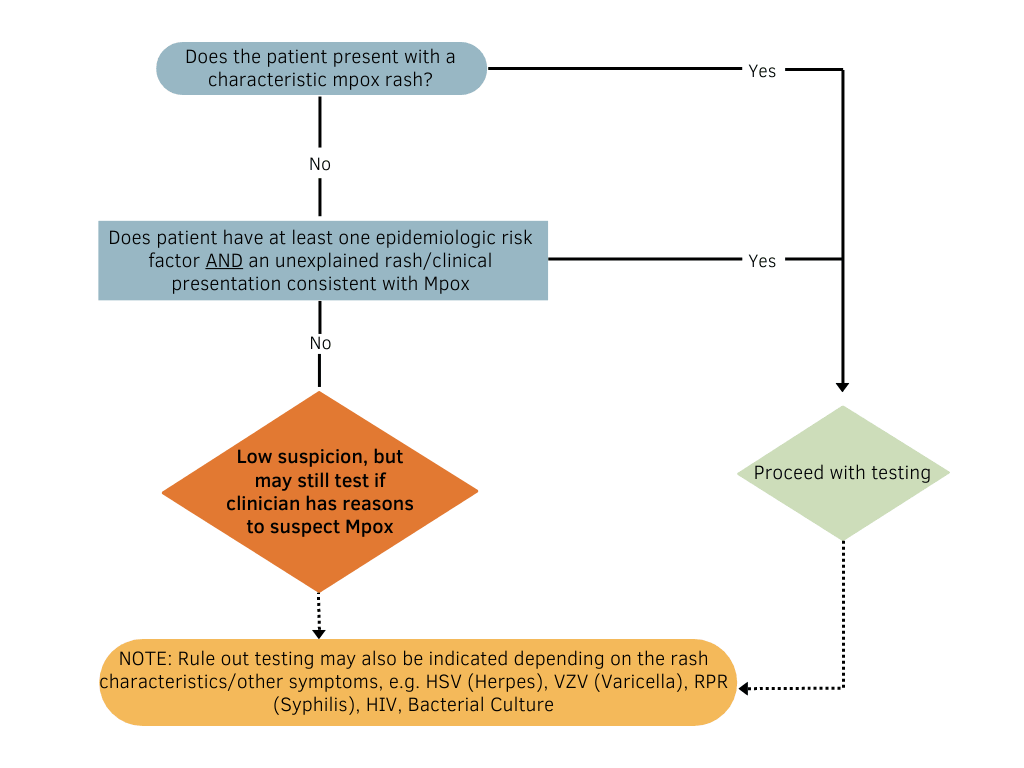
Decision Matrix
Treatment with Tecovirimat (TPOXX)
Tecovirimat (TPOXX) is an antiviral medication that is approved by the United States Food and Drug Administration (FDA) for the treatment of smallpox in adults and children. Data are not available on the effectiveness of Tecovirimat (TPOXX) in treating mpox infection in humans.
Consideration for prescribing Tecovirimat requires documentation and patient informed consent.
General Guidance for Tecovirimat Prescribers
Information for Obtaining and Using TPOXX
Required Documents for TPOXX Use:
- Informed Consent Form: English|Spanish
- Patient Intake Form
- FDA Form 1572
- Clinical Outcome Form
- PDF MedWatch Form for Serious Adverse Events
Vaccination
Stanislaus County receives Jynneos vaccine allotments from CDPH based on a formula using current mpox case counts and eligible population size. We continue to request as many doses as allocated in the shortest timeframe available to address the critical shortage of local vaccine needed to stem the outbreak. Information about the amount of Jynneos vaccine allocated to the county can be found at CDPH's Mpox Vaccine Page.
Vaccine supply has increased. Vaccines are now available for anyone who may be at risk and anyone who wants to get vaccinated.
Certain groups are especially recommended to get vaccinated. These groups are:
- Anyone living with human immunodeficiency virus (HIV), especially those with a CD4 count <350/mm3, an unsuppressed HIV viral load, or an opportunistic infection.
- Any man or trans person who has sex with men or trans persons
- People who use or are eligible for HIV PrEP
- Sex workers
- Sexual partners of the above groups
- People who have had direct skin-to-skin contact with one or more people AND who know others in their community that have had MPX infection
- People who have been diagnosed with a bacterial sexually transmitted disease (e.g., chlamydia, gonorrhea, syphilis) in the past 3 months
- People who anticipate experiencing the above risks
Individuals may be vaccinated in Stanislaus County even if they live outside of Stanislaus County.
Vaccine appointments are now available on myturn.ca.gov.
For more information regarding mpox Vaccination, visit CDC's Vaccine Clinical Considerations Page.
Infection Control: Healthcare Setting & Mpox
- Droplet precautions should be applied in all healthcare settings when a patient presents with fever and vesicular/pustular rash
- PPE should be donned before entering the patient's room and disposed of prior to leaving the isolation room. PPE includes
- Disposable Gown
- Gloves
- Eye Protection (i.e. goggles or a face shield that covers the front and sides of the face
- NIOSH-Approved particulate respirator equipped with N95 filters or higher
- Patient should be placed in an isolation room (negative air-pressure if available)
- If the patient is transported outside of their room, they should use well-fitting source control (e.g. medical mask) and have any exposed skin lesions covered with a sheet or gown
For more information please visit: Infection Prevention and Control of Mpox in Healthcare Settings.
Epidemiology of Mpox
Risk Factors for Mpox:
While anyone can get mpox, certain individuals are at higher risk of contracting mpox. This includes people who have:
- Had close, intimate contact with someone with a suspected or confirmed diagnosis of mpox.
- Touched unwashed materials that were exposed to the fluid present in the lesions including bedding, towels, or clothing.
- Had contact with bodily fluids of an infected person.
Certain individuals may also be at higher risk of severe disease, including:
- Immunocompromised individuals
- Pediatric populations
- Pregnant or breastfeeding women
- People with a history or presence of atopic dermatitis and people with other active skin conditions such as eczema, burns, impetigo, and varicella zoster virus infection.
How Mpox is Presenting in Current Outbreak:
- The current data show transmission is higher among people in close social networks.
- In current outbreaks people with mpox generally report having close, sustained physical contact with other people who have mpox.
- Painful herpetiform lesions on the skin and mucous membrane at sites of intimate contact.
Symptoms:
The Key Symptom is Rash or Pimple- or Blister-Like sores that may have these features:
- Sores are painful or itchy
- Sores go through multiple stages before healing. Individual sores may be in different stages
- Commonly found on or near genitals, anus, hands, feet, chest, and face
- May be found on multiple parts of the body or only one part
Other symptoms include:
- Fever
- Chills
- Tiredness or low energy
- swollen lymph nodes
- General body aches
By far, the most common symptom of mpox is rash and sores. Some individuals will experience all these symptoms, while others may only experience a few.
How long do mpox symptoms last?
- Symptoms usually start within 3 weeks of exposure to the virus.
- Rash 1-4 days after flu-like symptoms.
- Mpox can be spread from the time symptoms start until the rash has healed (typically in 2-4 weeks).
- A rash is considered healed when all scabs have fallen off, and a fresh layer of skin has formed.
Additional Resources
CDC's Information for Healthcare Professionals
CDC's Information for Laboratory Personnel
CDC's Information for Veterinarians



